More and more interesting questions keep coming up, unfortunately with a higher rate of new questions than definitive answers, but let’s dive in and see what we can come up with.
I’m in the “old age” and “high risk” category. Does this mean that if I go out, I will get the disease easier than someone else, or does it mean that if I get it, chances are it will be worse for me? I’d like to go out once in a while, but I feel like the virus will be “looking for me” as an easy target.
It’s easy to want to anthropomorphize this virus, but SARS-CoV-2 doesn’t care about anything. It is completely dependent on the activity of us to replicate and to spread. It’s not “looking” for anyone and doesn’t seek out high risk folks to come into contact with.
I think that your risk of being infected is dictated by contact with the virus and not your level of risk. Age and medical issues dictate a lot of your risk of severe illness once you’re exposed, and so you should take precaution when interacting with people accordingly.
Any again, I think I’ve said this in prior newsletters, but you can keep your risk - and the risk of those around you - low if you:
Wash your hands frequently
Wear a mask
Avoid close interaction in confined, crowded, and poorly ventilated spaces
Isolate if you have any symptoms and encourage others to isolate with symptoms
If health care workers can spend so much time working closely with these patients and have low risk of infection, it means that taking precautions works.
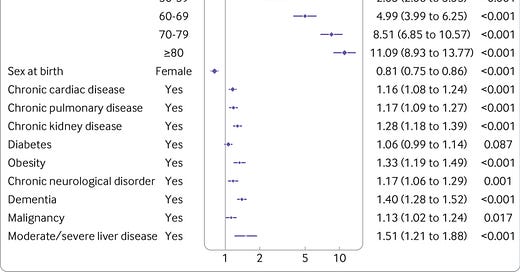
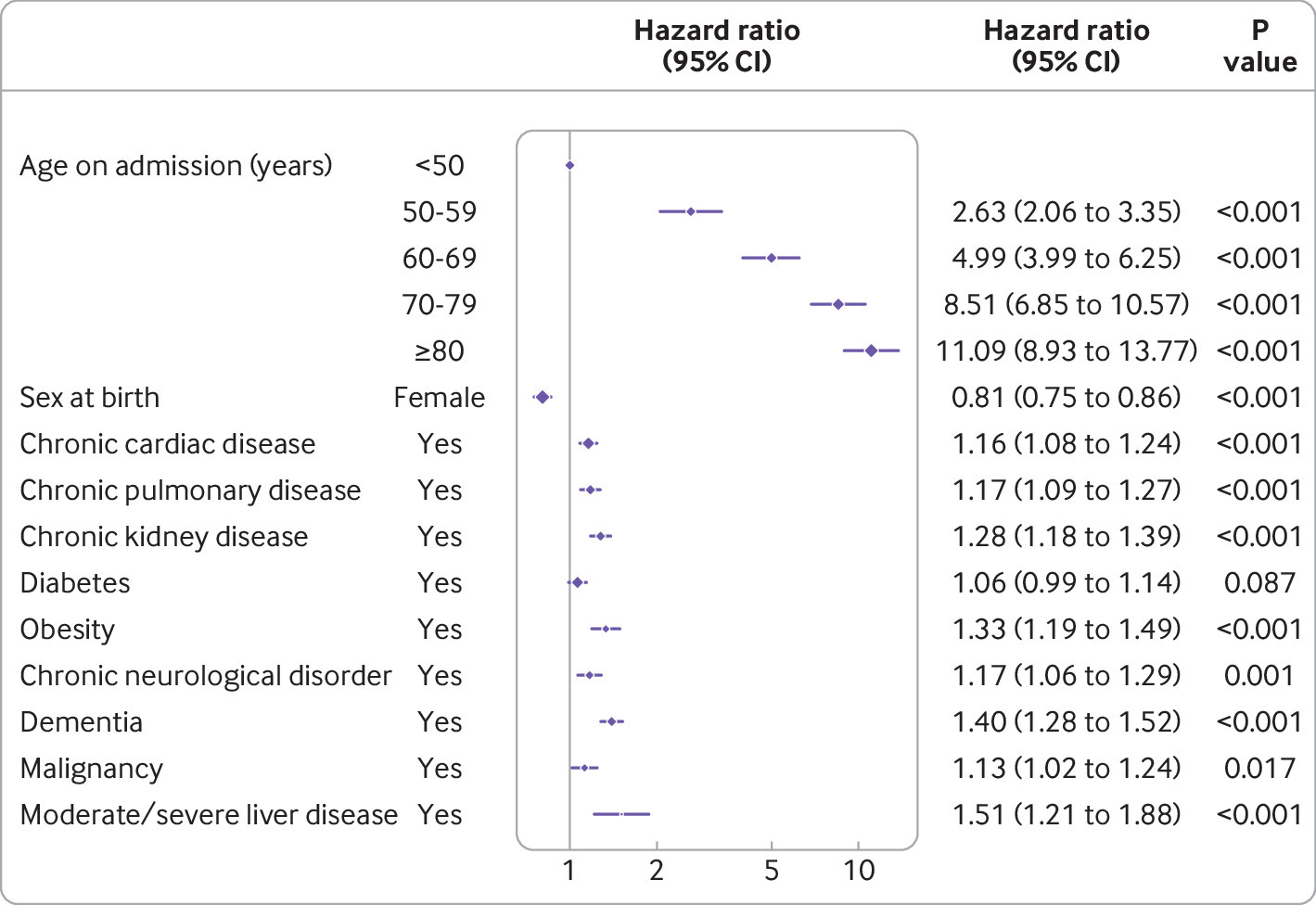
A new paper in the British Medical Journal looks at how much different risk factors are associated with risk of death. What you see when you plot out the numbers is that BY FAR the biggest risk factor is age. While things like obesity and chronic disease certainly have an impact, it’s marginal compared to age.
Take a look a this graphic. Hazard ratio refers to your relative chance of having an outcome in question - in this case the outcome is death.
Obesity gives you a hazard ratio of dying from COVID of 1.33, which means that you’re 33% more likely to die from COVID if you’re obese than a non-obese person.
But having an age between 70-79 gives you a hazard ratio of 8.51, which means you’re 851% more likely to die from COVID if you’re in that age range compared to someone under 50.
Why are more men than women dying from COVID?
It seems that no matter what metric you use - hospitalizations, deaths, need for a ventilator - men fare worse than women when it comes to COVID. Even when researchers use complicated statistical methods to adjust for other patient factors, they still seem to find that male sex is associated with worse COVID outcomes.
The leading hypothesis at the current time has to do with likelihood of the virus to enter our cells. Entry into a cell by the virus isn’t haphazard, it has to occur through a special doorway, which we call a receptor. The virus uses the ACE2 receptor to get into cells.
If you have more ACE2 receptors available, it means more portals for the virus to get into your cells.
Men seem to have higher levels of ACE2 receptors than women do. It’s unclear if this is dictated by estrogen, but there’s some research suggesting that it might be.
The reduced levels of ACE2 receptors might also be why children have less severe disease.
Wait, I heard about this ACE2 receptor. Should I stop taking my high blood pressure medications like I heard on the news?
There’s been a lot of smoke regarding high blood pressure medications and COVID risk. Similar to the gender difference, there’s thought that the ACE2 receptor comes into play here.
The levels of ACE2 receptors that we have is affected by two common classes of blood pressure drugs - ACE inhibitors and angiotensin receptor blockers (ARBs).
You might have heard of some of these medications - lisinopril, altace, diovan, losartan, etc. All ACE inhibitors end with “-pril” and ARBs end with “-sartan” (their generic names, not brand names) so you can use these clues to figure out if you’re on one.
So while we have a mechanism for an interaction between these high blood pressure medications and severity of viral infection, the actual relationship doesn’t appear to be that significant.
I wouldn’t make any changes to your medications on your own, and I’m skeptical that adjusting high blood pressure meds will have any impact on COVID. And if they do, it’s just as likely to increase risk as it is to decrease risk.
My friend will only get takeout that he can bring home and microwave before eating. Is microwaving effective for killing the virus on food?
Probably. But there isn’t something special about the microwave. Heating food in any manner likely kills the virus effectively.
As long as food has been prepared in a sanitary way and cooked appropriately, risk is of transmission is pretty low.
I’ve had the virus. You’ve said that I should continue to wear a mask, but for how long? Would I be able to visit people who are still in quarantine if it’s been more than a month since my symptoms?
No one knows about how long infectivity persists. Each time I dive into this topic, the information seems to change. Risk of infecting others drops the longer you’ve been asymptomatic.
Based on what I’ve been reading, I suspect that waiting two weeks after you don’t have any more symptoms of infection probably means you’re not contagious.
That said, I’m sure there will be outliers in this realm, and it never hurts to exercise caution.
I think that you can feel safe to start visiting two weeks after symptoms of infection have gone away, but would be mindful of who you’re with and what their risk is. When you’re around people over 60, it probably pays to take extra caution, just based on risk of severe infection.
I’ve said before that wearing a mask isn’t about you, it’s about those around you. It’s like returning a shopping cart - a slightly inconvenient, but easy-to-do behavior that is done primarily for the benefit of others.