"Do I really need that blood pressure medicine?"
Lessons from a huge clinical trial on blood pressure treatments
Every day of my life, I treat high blood pressure, and every day, I have patients asking me whether they *really* need to be on their medications.
High blood pressure (AKA hypertension) is incredibly common - I’m sure you know quite a few people who take medications for hypertension (and you may even do so yourself).
So the question of whether you really need to take blood pressure medications is relevant for many of us.
The relationship between high blood pressure and increased risk of heart disease has been known for decades and the treatment of hypertension is one of the cornerstones of preventive cardiovascular medicine.
As you can see below, the risk of cardiovascular events (AKA heart attacks and strokes) goes up as blood pressure goes up, with the lowest risk observed at a blood pressure of about 115/75:
So if the observed risk of cardiovascular disease starts going up when blood pressure rises above 115/75, should everyone with a blood pressure higher than that be on medications?
Before we get into the details here, one caveat I want to address. Blood pressure certainly responds to changes in diet, exercise, stress, sleep, sunlight, inactivity, and weight. By discussing medications I’m not avoiding these important topics, I’m merely saying that medications are a tool in the toolbox that we should think about when and how to use.
Deciding who to treat and when to treat hypertension is an important question to answer
After all, heart attacks, strokes, and congestive heart failure are all bad things. And if you can give people medications that are well tolerated and inexpensive to reduce that risk, it’s probably a good thing.
But most clinical trials address the question of treating very high blood pressures, not just mildly elevated ones.
Clinical practice guidelines don’t recommend medically treating blood pressure under 140/90 for most people who are otherwise healthy (of course, healthy diet and exercise are important, but let’s leave them out for the purposes of this discussion).
Many of my patients fall into the borderline range with a blood pressure that’s above the optimally observed value but below the value that mandates medical treatment - so they’re above 120/80 but below 140/90.
Do these borderline patients do better with blood pressure treatment?
This is the question that the SPRINT trial attempted to answer, and the results are interesting and informative enough that I think they’re worth discussing.
So how aggressively should high blood pressure be treated with medications? What can we learn from this trial?
Treating high blood pressure lowers risk of heart attacks, heart failure, and death
The SPRINT trial showed that even in low risk patients, the number of heart attacks, heart failure, and deaths were lower in a group treated more intensively than less intensively.
Let’s specify what “intensive treatment” means here.
The SPRINT trial took patients without heart disease or diabetes and put them into two groups:
Intensive treatment - goal blood pressure of under 120
Standard treatment - goal blood pressure of under 140
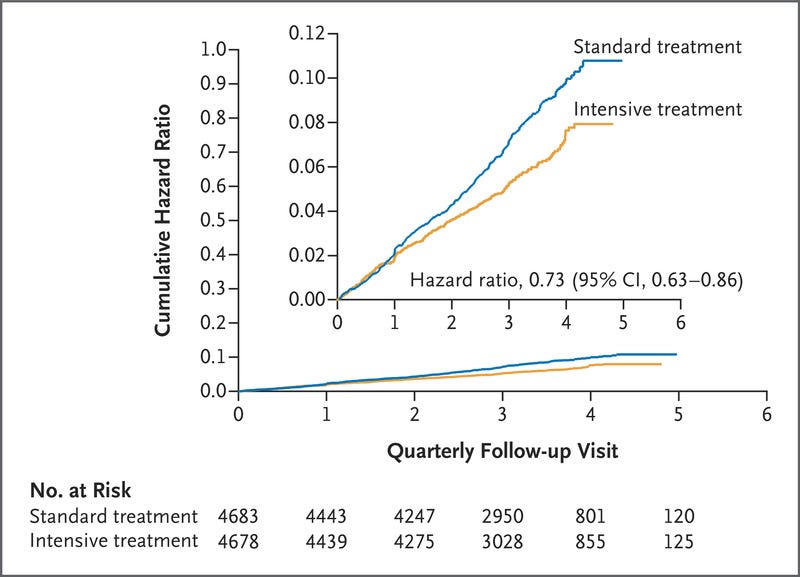
They found that the intensive treatment group had a lower risk of heart attacks, heart failure, and death, and that the differences between the groups were increasing over time:
So is that the ballgame?
Does this mean that everyone who has a blood pressure over 120 should be treated with medications?
In real life, it’s always a more complicated decision
As with any subject, when you dig into the details a bit more, you get additional information that may change your opinion.
I think it’s worth pointing out a couple of things in this study that color my interpretation of the results.
The actual incidence of bad outcomes in this study and the magnitude of improvement with more intensive hypertension treatment
The real world impact is likely overestimated because of mandated step-down therapy in the standard treatment group
The ongoing separation of the curves over the years, suggesting a cumulative benefit with longer term blood pressure treatment
Let’s look at each of these in a bit more detail.
Intensive treatment only lower risk by a small amount
First, the absolute incidence of bad outcomes in this study were low and the absolute decrease in rate of important events was incredibly low.
Look at the numbers here:
Heart attacks occurred in 0.68% of patients per year in the intensive treatment group compared to 0.93% per year in the standard group. That means risk of heart attack was cut by about 0.25% per year in absolute terms.
Risk of heart failure had even lower numbers - 0.45% in the intensive group versus 0.70% in the standard group.
Death was 1.06% per year in the intensive group and 1.41% per year in the standard group.
So, yes, it is completely true that the numbers are lower with intensive treatment. But they aren’t that much lower.
In other words, you’re probably going to be fine with either treatment approach, although risks do go down a little bit with more intensive therapy.
The real world impact is probably even lower than the trial suggests
If you read the supplementary appendix in this trial, you see that the trial protocol differs from how many people practice medicine in real life.
The protocol mandated that people who had a blood pressure under 130 in the standard group had a step down in their treatment. If you came for follow up with a single blood pressure reading of 129/80, you were taken off medications even if you were feeling well and not having any side effects.
The reason that the trial designers did that makes total sense - if you want to see whether treating blood pressure more aggressively makes outcomes better, you need to make sure that there’s really a difference in blood pressure between the groups.
So if a patient in the standard treatment arm is treated to the point that their blood pressure is the same as a patient in the intensive treatment are, you may not see a difference with an intensive treatment strategy.
If you’re trying to answer a research question, that design makes sense - you want an actual difference between the groups.
But in real life, if a patient comes into my office on blood pressure medications and is doing well with a blood pressure that’s controlled, I usually don’t stop their meds because the medications are doing what they’re supposed to do.
So in a trial that forces a de-escalation of treatment, you’re probably going to have more heart attacks and heart failure as a consequence of higher blood pressure from taking away medications.
That means the impact of intensive treatment is probably over-estimated by this study and the actual difference between the groups is even less in the real world.
The benefit of high blood pressure treatment compounds over time
When I read papers, I’m always obsessed with the shape of the event curves over time because it tells me about the natural history of the process that we’re investigating.
The intensive treatment group curve has a different slope than the standard treatment group and that the difference between the curves is increasing over time.
That difference suggests an ongoing treatment effect that may get larger over more time. This study only followed people for 5 years, suggesting that the long term impact of better blood pressure treatment may be underestimated.
Considering that most people are diagnosed with high blood pressure many years before a heart attack, the long term impact here is vitally important because it may change the way that we approach blood pressure control.
So what’s the bottom line?
My take away here is simple: lower blood pressure reduces risk of cardiovascular disease and the impact of lower blood pressure on outcomes increases over time.
It doesn’t mean that I’m throwing all my patients with minimally elevated blood pressures on tons of medications that they take forever.
Rational people can look at this data and draw different conclusions. I don’t know how much the treatment effect size is overestimated based on the trial protocol or whether the long term impact of treating blood pressure attenuates over time.
And most people would prefer to be on fewer rather than more medications.
So if your blood pressure is over 140/90, the answer is easy - if you aren’t making major changes to your diet, exercise, sleep, and stress, almost everyone should be on medications.
When your blood pressure goes below that level, it becomes a more nuanced discussion - how old are you? What’s your cardiovascular risk? Do you have other medical problems? What’s your risk tolerance? How much do you hate taking medications?
At the end of the day, it’s an individual decision and what’s right for me might not be right for you.
Thank you for reading! If you’re enjoying my newsletter, please share on social media and encourage your friends and family to subscribe!