Podcast: why don't we use the best biomarkers?
A discussion on kidney function and how to measure it better
One of the things that’s hardest to deal with in medicine is the uncertainty of testing.
Sometimes that uncertainty happens in the form of a false positive or a false negative.
But something that uncertainty happens because we aren’t using the best test to answer the question that we want.
You’ve probably had bloodwork done that checked a marker called creatinine, which is then used to estimate your kidney function.
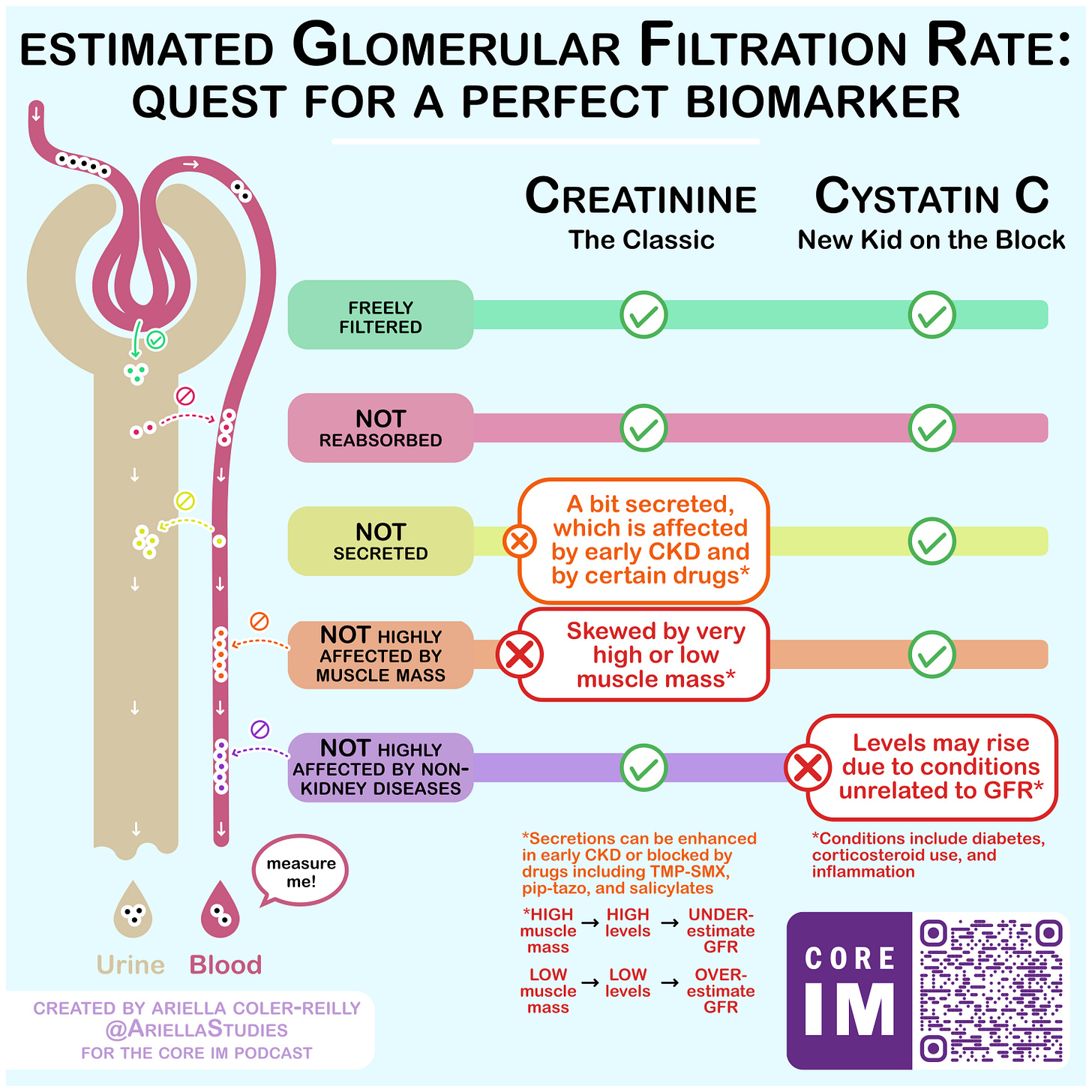
It turns out that creatinine a suboptimal biomarker to assess kidney function with a lot of reasons it can give a falsely high or falsely low value.
And moreover, the thing that creatinine is trying to inform us about - glomerular filtration rate, or GFR - isn’t the best way to figure out who should be on medications for slowing the progression of kidney disease.
I did a podcast recently asking some questions about the way that we measure kidney function and how we might be able to do it better.
Take a listen - it’s under 30 minutes long and packed with information:
We covered topics like:
Why just looking at GFR often misses important information about kidney function and why assessing protein in the urine (microalbuminuria) is a vital component of understanding kidney disease
The common problems with using creatinine to measure kidney function and the ways that it can mislead us
Introducing a better biomarker for kidney function - Cystatin C
A detailed discussion of protein in the urine as a prognostic sign and a marker of who merits treatment
Show notes and transcript can be found here.
A graphic discussing advantages and disadvantages of both creatinine and cystatin C: