Blood clots in COVID are a real thing. We’re seeing all kinds of weird clotting events happen in these patients when they’re sick enough to be admitted to the hospital.
I’ve seen COVID patients with blood clots in their large veins (deep vein thrombosis, or DVT) and blood clots in their lungs (pulmonary embolus or PE).
COVID patients with kidney failure are developing clots in their dialysis catheters.
I’ve seen real heart attacks in patients with active COVID infection.
Some of the sickest COVID patients are even developing blood clots despite being on high doses of blood thinners.
And autopsies of COVID patients demonstrate tiny blood clots in the lungs, kidneys, and other organs, suggesting that clotting may be behind some of the organ failure we’re seeing.
What is going on here?
Blood clotting happens because of disturbances in one of three different areas, termed Virchow’s triad, which are: stasis of blood flow such as what occurs with prolonged immobility, increased activation of the body’s own coagulation system (hypercoagulability), and injury to blood vessel walls (endothelial injury).
All 3 areas can be affected in COVID-19 and no one fully understands exactly why these patients seem to be having such profound and pathologic blood clotting. But we know that the sickest patients are the ones who have the worst clotting problems and that those with minor disease tend to have lower risk.
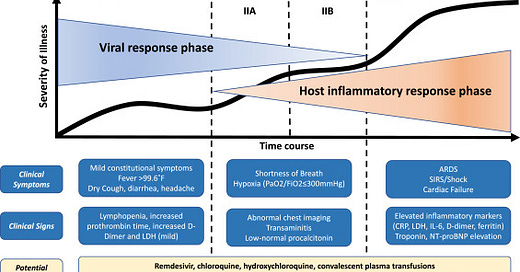
Severe COVID-19 infection seems to have 3 different phases: early infection, pulmonary phase, and then a hyperinflammatory phase.
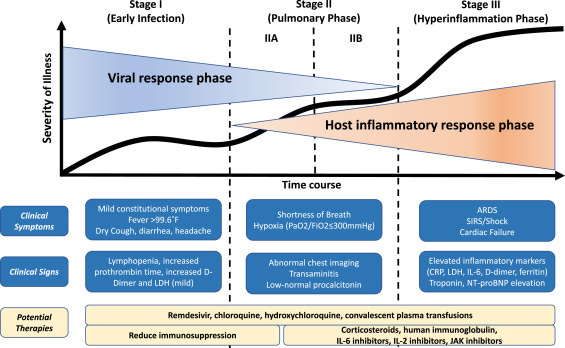
The hyperinflammatory phase is when we see clotting problems. We suspect that during this phase, the body’s response to the virus is causing more problems than the virus itself. This is similar to an autoimmune disease, where an overactive immune system causes symptoms, but in the case of COVID-19 it’s an overreaction by our immune system to the threat of the virus.
There’s an interaction with the immune system and the coagulation system, which some have termed “thromboinflammation.” It’s hypothesized that our body’s immune response to COVID is largely responsible for the increased blood clotting that we’re seeing.
Why are you annoying me with so much biology?
Understanding the mechanism of disease is a vital part to coming up with ideas about how to treat it. The research on physiology sets us up to ask questions that we can test in clinical trials to figure out if treatments work.
I’m focused on the biology here because there are different types of blood thinners that we can give to patients depending on which part of blood clotting is impacted.
The two major components of the coagulation system are platelets and coagulation factors.
If the problem is with overactive platelets, we would treat with medications like aspirin or clopidogrel. If the problem is with overactive clotting factors, we would treat with medications like heparin or enoxaparin.
Autopsy studies of these patients suggest that both platelets and coagulation factors appear to be activated in severe COVID infections, so the possibility of using medications to inhibit both pathways is intuitively appealing to me.
What should we do about these clotting problems?
Most people who get infected with COVID aren’t going to have problems with blood clotting. The average person who gets infected shouldn’t take blood thinners when they’re at home unless prescribed for other reasons. It’s almost certainly a mistake that just puts you at risk of bleeding complications without providing any clear benefits.
The trickier question that we’re confronting daily is what to do about patients with severe disease. We trend different laboratory markers of blood clotting while patients are in the hospital, looking at the change in these values on daily bloodwork. We know that there is a significant relationship between patients who have very high lab markers of blood clotting and those who develop blood clots.
As a consequence, a lot of hospitals are developing protocols for empiric anticoagulation (empiric meaning based on an educated guess rather than observation of true disease) based on levels of a marker in the blood called a D-dimer when patients have no evidence of blood clots.
This is controversial. We know that blood thinners have well described risks - internal bleeding, intracranial bleeding - and there isn’t a clear benefit of being on a blood thinner if no blood clot can be observed. But the levels of blood clotting that we’re seeing are so profound and so disturbing that a lot of really smart people think that preventively giving these medications is the right thing to do.
What about medicines that break up blood clots?
The Associated Press recently published an article on an emergency room doctor at Mount Sinai who was using a medication that breaks up blood clots in the treatment of patients with severe COVID-19 infections. This got picked up by media outlets all over the country - the New York Times, Washington Post, Los Angeles Times.

The article tells the story of an emergency room doctor at Mount Sinai who started giving a medicine called tPA, a blood clot busting medication, to patients with severe COVID infection. We typically only use this medication in a handful of clinical scenarios: an active stroke, a major heart attack when we can’t perform a catheterization, or a life threatening pulmonary embolism.
tPA has real risks of bleeding. You only need to take care of one patient who gets tPA and has a catastrophic bleed inside their skull to have it change the way you practice medicine.
I think that promoting this type of treatment - and the doctor who decided on it - as heroic is probably wrong. Around 80% of the patients sick enough to try these interventions on are going to die. In fact, the patient referenced in the article passed away, so this treatment actually didn’t even save a life. Suggesting the promise of this treatment as potentially life saving is questionable, at best.
So what’s the bottom line?
As I’ve said before, we need well run clinical trials to guide therapy in COVID patients. In many ways, because the really sick patients are doing so poorly, COVID has turned medical care into the wild west, where many feel license to indulge their pet ideas on disease treatment into experimenting on patients, most of whom are going to die anyway when they’re sick enough to be intubated. The only way to really decrease the probability that we’re causing harm to patients through these “gambles” is by studying what works and what doesn’t.
When we’re treating these patients, we need to look thoroughly and proactively for blood clots in patients who aren’t doing well so that we can treat them. We need to monitor the effectiveness of therapy and adjust if it’s not good enough.
I’m advocating for ramping up clinical trials of different blood thinning strategies in COVID patients. We should be asking tough questions and studying things quickly to develop treatments to help these patients. But gambling on treatments because we read about them in the media is a risk I’m unwilling to take.