Have you ever heard of a risk calculator?
It’s one of the most common tools that doctors use to decide on heart disease treatment that doesn’t get a lot of press.
A risk calculator is similar to what it sounds like - a method of estimating the risk of a heart attack or stroke based on a patient’s demographics and medical history.
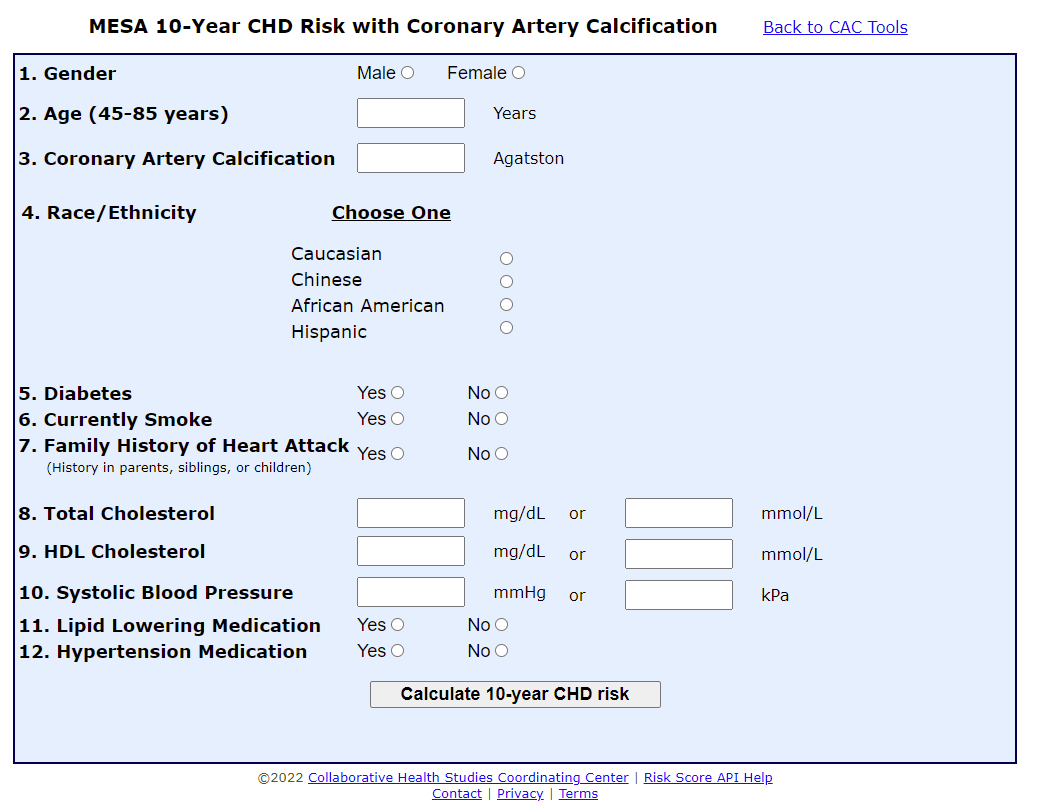
There are a handful of well known calculators out there - the ACC/AHA calculator, the Framingham risk score, the Reynolds risk score, the MESA calculator - that each estimate cardiovascular risk over a 10 year horizon.
They’re all simple to use and easily available online. Here, take a look:
While these calculators are great - and I certainly use them frequently! - they aren’t perfect, and some patients fall through the cracks.
There are two major flaws with these calculators:
They don’t take into account all of the risk factors for cardiovascular disease, so you underestimate risk in people with medical issues that aren’t captured by the calculators.
The risk that comes out of these calculators is driven by predominantly by age. That means that lifetime risk in young people is underestimated (sometimes by quite a bit). As a result, we miss opportunities to treat people who would really benefit from treatment over the long term.
So if you’re only going by standard measurements of risk, you wind up under-treating some vulnerable people (and possibly over-treating some older, less vulnerable people).
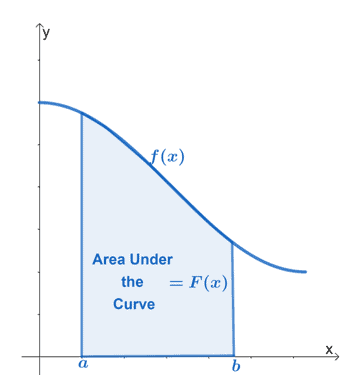
Heart disease risk is all about area under the curve
You can’t think about heart disease accurately without implicitly considering some math. And before you see the graph below and stop reading, I promise that it’s relevant and doesn’t require any hard thinking.
No one is reading this newsletter because they have any interest in calculus, but communicating about this concept is vital to how I think about heart disease.
It’s not just the presence or absence of a risk factor that matters. It’s also how long it’s there for and how poorly controlled it is.
Take high blood pressure. The higher your blood pressure is and the more years it’s elevated, the higher your risk of heart attack and stroke
Take diabetes. The longer you’ve had diabetes, the more insulin you need, and the less your blood sugar is controlled, the more likely you are to have a cardiovascular event.
The same is true for cholesterol, smoking, or any other risk factor you can think about.
Exposure * Time = Risk.
So risk factors at age 40 may not cause problems by age 50, but there’s a really high chance that they’ll cause problems by age 60 or 70. And considering this in terms of lifetime risk better captures the right way to think about heart disease.
The other huge problem with the risk calculators: they miss people with “non-traditional” risk factors
While the standard method of risk factor assessment - smoking, diabetes, cholesterol, high blood pressure, and family history - certainly tells us a lot, it doesn’t tell us everything.
There are a handful of additional important questions about medical conditions that don’t ring the standard alarm bells that need to be asked if you want to truly personalize cardiovascular disease prevention.
Preeclampsia, PCOS, premature menopause
We do such a bad job of preventing and treating heart disease in women that there’s a whole month dedicated to doing better each year.
When I see a female patient for a preventive evaluation, taking a good obstetrical history is of vital importance for better understanding personalized cardiovascular risk.
Things like preeclampsia, eclampsia, HELLP syndrome, polycystic ovarian syndrome, premature menopause, infertility, and early or late menstruation all influence cardiovascular disease risk.
Not recognizing these conditions as cardiovascular disease risk factors is certainly a part of why women have worse outcomes with heart problems than men do.
You won’t find anything about women’s health in the risk calculators.
Chronic kidney disease
Patients with abnormal kidney function aren’t just at higher risk of cardiovascular disease, they are also more likely to present to medical attention with non-classical symptoms or sudden death.
And when it comes to kidney disease, it isn’t just that these patients are more likely to have diabetes and hypertension than other patients.
Kidney disease by itself causes an acceleration of heart disease via inflammation, oxidative stress, and abnormal calcium metabolism.
Patients with chronic kidney disease can often have symptoms of a heart attack that don’t fit our typical narratives for what people experience. Less than half of patients with kidney disease have chest pain when they have a heart attack - it’s common to have shortness of breath or fatigue as the only presenting symptom for these patients.
None of the risk calculators incorporate kidney disease.
Autoimmune disease and chronic infection/inflammation
Patients with autoimmune diseases like lupus, rheumatoid arthritis, and inflammatory bowel disease are more likely to have cardiovascular disease than their age, sex, and risk factor matched peers.
This is probably related to the fact that these disorders are associated with low levels of chronic inflammation and inflammation plays a major role in heart disease pathogenesis.
You should also include patients with chronic infections, particularly HIV, as having a higher than expected risk that isn’t going to be captured by any risk calculator.
Lp(a)
I’ve written before in this newsletter about the importance of Lp(a) in the development of heart disease. Elevated Lp(a) is often the culprit in families where everyone gets bypass surgery or has a heart attack before they’re 40.
I don’t need to belabor it, but you can read more here if you’re interested.
Lp(a) isn’t in any of the standard risk calculators, but it is one of the biggest risk factors that gets missed if you don’t know to check it.
Metabolic syndrome
This one actually sort of makes its way into the risk calculators when they ask about HDL-cholesterol and blood pressure.
Metabolic syndrome can be thought of as pre-pre-diabetes, but it’s a huge part of chronic disease risk.
Metabolic syndrome is generally defined as having 3 out of 5 of the following findings:
Abdominal obesity
Elevated triglycerides
Low HDL cholesterol
High blood pressure
High blood sugar
It’s worth emphasizing that if you have signs of metabolic syndrome, your heart disease risk is higher than it should be.
In summary - don’t neglect the “non-traditional” risk factors and don’t mistake medium-term risk for lifetime risk
Knowing the limitations of a tool is vital to being able to apply it well.
The cardiovascular disease risk calculators that we have are great tools, but they miss a lot of important factors that play a role in the development of heart disease.
By understanding your own risk factors well, you become empowered to bring them up with your doctor and advocate for yourself.
Thank you for reading! Please share on social media and encourage your friends and family to subscribe!