The two biggest errors in COVID risk assessment
Humans are bad at assessing risk.
Even if I wasn’t fully persuaded by the extensive research on this before the pandemic, the COVID experience has led me to be certain that it’s the case.
Of course, not all risk is created equal, and the potentially civilization-ending tail risk of a contagious respiratory virus is different than the individual risk of not wearing a seatbelt or deciding to smoke.
But, as I’ve mentioned before, I’m not a sociologist, I’m a doctor. And while the evolutionary benefit of our skewed risk assessment is certainly interesting, it’s not necessarily an area that I have much to add to.
From my patients along with my family and friends, I’ve observed two major flaws in COVID risk assessment when it comes to the pandemic that I thought would be worth sharing here.
The first major error in COVID risk assessment: not understanding effect size
Every doctor knows that there’s often a gap between your perception of the importance of a medical intervention and the perception that your patients have of the same intervention.
I don’t think I fully appreciated the extent of this gap until seeing some of the chaos around interventions to treat and prevent COVID.
A big part of the reason why so many people are taking ivermectin (and getting sick from it) and why hydroxychloroquine is still part of the COVID culture wars is that there’s an implicit assumption that these treatments are lifesaving for those who take them.
After all, how many people would be requesting ivermectin prescriptions (or buying it without prescriptions) if the optimistic case for response to treatment is that it gets rid of their mild COVID symptoms a day earlier?
I’ve written before about the concept of a parachute intervention (detailed extensively in the medical literature here) - something so obvious and with such a massive benefit that it doesn’t need to pass muster before being widely used.
Almost no medical interventions are like that. The best treatments that we have don’t actually have that massive an impact on your risk of dying from disease.
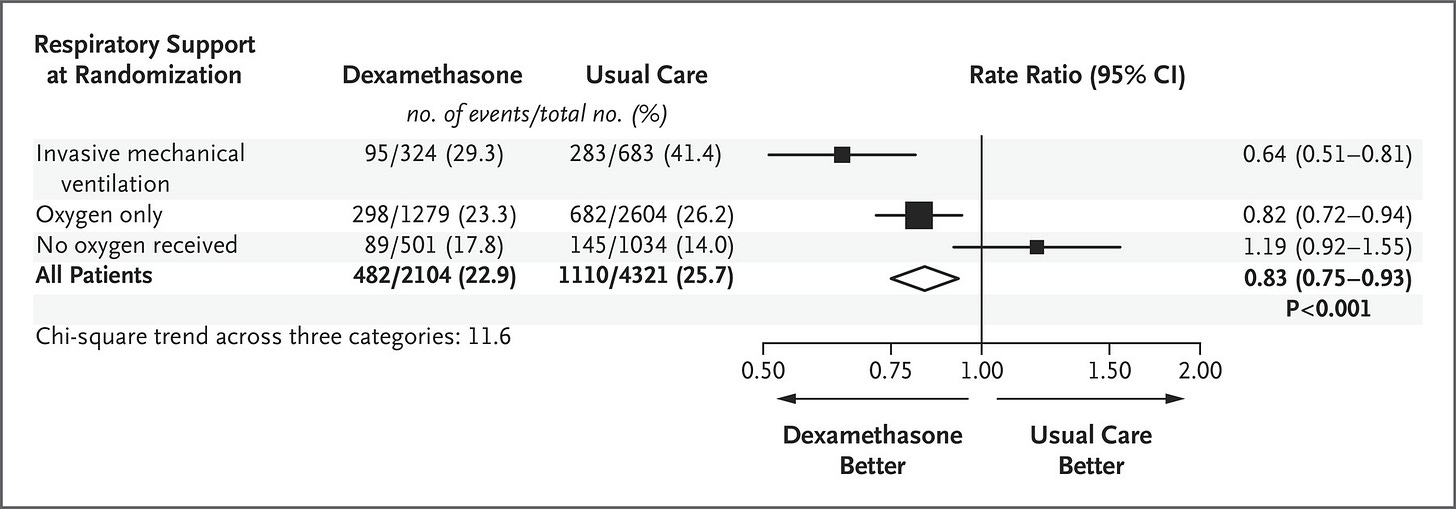
Take dexamethasone for example. Even the best treatment that we have for severe COVID changes the risk of death for patients on a ventilator from 41.4% to 29.3%. And for all hospitalized patients with COVID, risk of death is only decreased from 25.7% to 22.9%. Take a look:
So while this is a big deal - and I want dexamethasone if I get really sick with COVID! - this doesn’t save the life of everyone who takes it.
Take remdesivir as another example. The most optimistic reading of the clinical trial suggests that remdesivir reduces risk of death from 15.2% to 11.4% - a major benefit, incredibly impactful, but still, not a parachute. The effect size isn’t huge.
The most generous reading of the medical literature on things like vitamin D, zinc, hydroxychloroquine, and ivermectin is that they make a tiny impact on the margins of COVID and have no real impact on your risk of death or severe illness.
The same thing is true for convalescent plasma. Even monoclonal antibodies, which help against COVID, don’t help that much.
And community mask wearing - a topic worth a bigger deep dive in the future here - may not have as massive a benefit as we hope that it will.
In medicine, we often use a concept called the “number needed to treat” to quantify how impactful an intervention is. It’s an estimate of how many patients you treat with a medication to impact one patient.
The NNT for dexamethasone in intubated patients is about 8. That means for the best intervention that we have for COVID, you need to treat 8 patients to save 1 life.
The NNT for a parachute is about 1 - you need to treat one skydiver with a parachute to save one life.
The other major risk assessment problem that I’ve seen: not focusing on the things you can control
You may have heard the COVID wave that we’re currently experiencing described as “a pandemic of the unvaccinated.”
While this is true - the vast majority of people currently dying from COVID are unvaccinated - it’s also incomplete.
The entire COVID experience has been a pandemic of the elderly, the underserved, the metabolically unhealthy, and those with chronic disease.
While we can’t change our chronological age, our parents, our race, or our socioeconomic status, we have a huge amount of control over our metabolic health and on chronic disease.
The vast majority of chronic disease is preventable (or curable) through changes to our environment - our diet, our physical activity, our sleep, our stress management, our sunlight exposure, our socialization.
Our medical system has many flaws, but perhaps the biggest one is the normalization of accumulating a growing list of medications for the treatment of chronic disease as we get older.
Although this has been normalized, it isn’t normal. For most people, a growing medication list reflects a mismatch between the environment that we live in compared to the environment that we evolved to live in.
By environmental mismatch, I mean the discrepancy between what we eat, how (and how much) we move, how much (and how well) we sleep, how much natural sunlight we get, and how we socialize with the way that we should be doing all of these things.
If you’re scared of COVID - and I know from the responses I get to this newsletter that many of my readers are scared - the two most important things that you can be doing to mitigate your COVID risk are:
Get vaccinated
Get as healthy as you possibly can
I’m not writing about this to start an argument about all of the life factors that stand in the way or the tragic socioeconomic and racial disparities that exist in this realm.
I fully recognize that there are some people who have life circumstances that make a healthy diet seem impossible/unaffordable or have too much to do at work and as a caregiver to find time to exercise. Many of these folks will also have chronically high levels of stress brought on by external circumstances and interrupted sleep due to shift work or a caregiving role.
I’m certainly not suggesting that this applies to everyone (although I think it applies to most).
But if you’re afraid of getting COVID and you aren’t eating less junk food and getting more exercise than you were at the beginning of the pandemic, you should consider this a huge missed opportunity.
Keeping up with the news on COVID treatment, local test positivity rates, and mask mandates are unproductive activities. Going to bed early, spending time with your friends and family, going for a walk outside, lifting weights, cutting down your sugar intake, and throwing out your junk food are productive.
As we move towards a time of endemic COVID, focusing on the things that we can control is going to become increasingly important.
Thank you for reading! Please share on social media and tell your friends and family to subscribe!