Last week, I wrote about how much we can learn from the cholesterol skeptics about heart disease. Many of these folks have certainly been influential in my own thinking.
To recap what I think they emphasize well for us:
There’s more to heart disease than just LDL cholesterol
Insulin resistance is a really big deal, and it’s underemphasized by most physicians
Doctors overprescribe medications and often use medications in situations when lifestyle changes are more appropriate
The public health community has gotten a ton wrong about heart disease, particularly about nutrition
When the government gets involved in nutritional policy, it ends up being a net negative for everyone who doesn’t hold stock in Big Food, Big Ag, and Big Pharma
But I also think they’re wrong when it comes to LDL cholesterol. Let me make the case for why that’s wrong.
First, a quick digression on definitions
LDL cholesterol is a confusing term. LDL stands for low density lipoprotein, and LDL cholesterol is often referred to as the “bad cholesterol,” a silly name that essentially means nothing. The cholesterol in LDL is the same as the cholesterol in HDL. Cholesterol is cholesterol, and the “good” and “bad” part is a bit of a misnomer.
Cholesterol is a molecule that every cell in our body needs to function. It’s used in cell membranes, to make hormones, and without cholesterol, we would die. But since cholesterol doesn’t dissolve in water, it needs to be carried through the blood by proteins.
The particles made up of proteins and cholesterol (along with triglycerides) are named lipoproteins. Lipoproteins have a variety of vital functions throughout the body. We literally can’t live without lipoproteins. LDL is just one type of lipoprotein.
But LDL is important to us in this story because it’s the major lipoprotein that can get stuck in the walls of a blood vessel and cause problems there when it incites inflammation and leads to a buildup in that blood vessel.
This disease process is known by many terms in the medical world: atherosclerosis, coronary artery disease, atherosclerotic cardiovascular disease, arteriosclerosis, heart disease, and so on. For all intents and purposes, these terms mean the same thing.
I wrote in a previous newsletter installment about the fact that the standard LDL cholesterol metric that you get on a normal cholesterol blood test sometimes isn’t all that helpful.
But the view of the cholesterol skeptics that markedly high LDL levels are meaningless and nothing to worry about is wrong. Let’s look at why.
The people born with genetic variants that lead to very high LDL cholesterol levels develop premature cardiovascular disease
Patients who are born with very high LDL cholesterol levels due to a condition called familial hypercholesterolemia (or FH) develop early heart disease.
FH can occur due to a variety of genetic variants, but the common thread among them is that LDL cholesterol levels (and levels of the total number number of LDL particles) are incredibly high.
Total cardiovascular risk in these patients is proportional to how high their LDL cholesterol is. You can be born with either one or two genetic variants here - the people who are born with two have much higher risk of premature heart disease.
Risk increase in FH is not trivial: we’re talking at least 5 times higher risk of a cardiovascular event in a patient with FH compared to someone without it.
Patients with untreated FH can develop cardiovascular disease in young adulthood. When you see a family that has multiple members who have heart attacks or require bypass surgery at a young age, FH is on the list of possibilities.
There’s an advocacy organization called the FH Foundation that is devoted to bringing attention to these vulnerable patients to improve early detection and treatment.
If you want to say LDL isn’t important, you need an explanation why patients with FH are at such high risk of premature cardiovascular disease.
The converse: genetic variants with very low LDL cholesterol are protective against heart disease
There are a number of genetic variants that have been discovered that lead to very low LDL cholesterol and a lifelong major reduction in cardiovascular events.
Take a look at a few:
PCSK9 loss of function leads to low LDL levels and a very low incidence of heart disease
Genetic variants that reduce function in the NPC1L1 receptor also lead to low levels of LDL cholesterol and protection from heart disease
Same story for HMG-CoA-reductase variants
The fascinating thing about the genetic variants and LDL story is the degree of risk reduction seem to be much more than you’d think based on the amount that LDL cholesterol is lowered.
This gets to the idea that we should think about LDL related cholesterol risk based on levels multiplied by time. This is a story where your risk is related to area under the curve, rather than just level.
The concept of heart disease being the result of cumulative exposure is vital to understand. We need to be thinking about this in terms of overall exposure, not just about the snapshots in time we look at when we check bloodwork.
When you look at the story of some of the LDL lowering genetic variants that confer protection against heart disease, it certainly persuades some doctors that we should be even more aggressive when it comes to medical treatment that we already are.
Lowering LDL cholesterol with medication reduces heart attack risk
The story here is the same across many different classes of drugs. Medical therapy to prevent heart disease in patients with elevated LDL cholesterol levels is safe and effective.
And it’s not just about statins, although it’s partly about them.
Look at ezetimibe.
Look at PCSK9 inhibitors.
Now, some of the cholesterol skeptics will point out a concerning item in the FOURIER trial. This was a trial of a PCSK9 inhibitor called evolocumab (also known as Repatha). If you look closely at the results here, you’ll see that more people in the evolocumab group died than in the placebo group.
This is concerning - don’t get me wrong. But I suspect it’s more an issue with the drug than with the concept of LDL lowering.
The ODYSSEY trial showed a reduction in death (in addition to a reduction in heart disease) using a different PCSK9 inhibitor called alirocumab (AKA Praluent).
At this point, the story is clear: when you have a safe drug that lowers LDL levels, cardiovascular disease risk appears to go down.
In summary: LDL matters, but it isn’t the only thing that matters
At the end of the day, I’ve been really influenced by the cholesterol skeptics in a positive way. I think I’m a better doctor for having been exposed to these arguments.
I think about heart disease in a holistic perspective, and I always try to address lifestyle in my patients.
But there’s a big problem with just throwing LDL out entirely as a risk factor - it ignores a lot of evidence that points to the fact that LDL does matter.
And it’s vital to remember that in a patient who has had a heart attack or stroke, you’re using an all-hands-on-deck approach to preventing another one - diet, exercise, sleep, and medications all play a role.
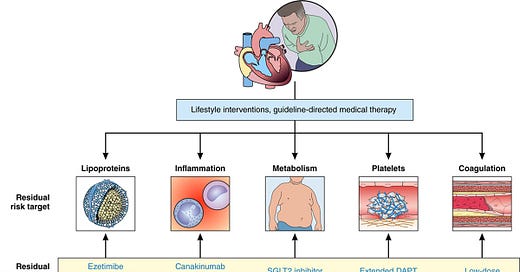
There’s a concept in cardiovascular disease prevention called residual risk that’s I’m fully persuaded is the future of personalized cardiology. It involves thinking about each patient’s heart disease as multifactorial and recognizing that there’s more to heart disease than just LDL cholesterol:
So at the end of the day the cholesterol skeptics teach us a lot. But I’m pretty sure that they don’t know everything there is to know about heart disease.
Thank you for reading! Please share on social media and encourage your friends and family to subscribe!