Which COVID vaccine is the best?
Now that we know the COVID vaccines are real and that they’re spectacular, the issue of whether you should get vaccinated becomes easy: of course you should. At least I think so.
But the next question is harder: which one should you pick?
For many of us, there isn’t really a choice, you’re going to sign up for a vaccination appointment and you’ll be given a whatever vaccine is available. But some of you may have a choice between the three different vaccines available.
So if you have the option to pick between Pfizer, Moderna, and Johnson & Johnson, which one should you choose?
Let’s start by reviewing the data here. We care about effectiveness, of course, but side effects and ease of dosing also matter. And with increasing concern about new variants, how the vaccine protects against the British, South African, Brazilian, and New York variants matters too.
(As an aside, I’m aware that there’s a bit of a backlash about naming these variants based on where they came from, so I’ll try to stick with B.1.1.7, P.1, B.1.351, etc moving forward.)
All of the vaccines are really amazing. But they aren’t perfect.
It’s easy to look at tables of vaccine efficacy from the clinical trials and conclude that it’s impossible to be hospitalized with COVID and impossible to die of COVID after you’ve been vaccinated:


While this table is great to see, it doesn’t actually tell us all that much. I’m not saying that it isn’t good news, just that it’s the tip of the iceberg.
For one thing, you can be really sick from COVID and not end up in the hospital. Plenty of people can have weeks of shortness of breath requiring self-proning to maintain adequate oxygen levels. So the trials don’t totally capture prevention of significant disease.
But more importantly, the trials weren’t designed to test the ability to prevent you from getting hospitalized with COVID. The trials were designed to test whether the vaccines protect against symptomatic infection.
Clinical trial design matters more than you might think here.
Since only a small number of people who are infected end up with symptoms, and only a small number of people with symptoms become sick enough to go to the hospital, and only a small number the patients in the hospital end up getting intubated or dying, we end up with really tiny number of patients in these trials who got really sick.
So when you look at the table above, you should remember the number of patients who were hospitalized in the placebo groups:
5 patients in the Pfizer trial were hospitalized
3 patients in the Moderna trial were hospitalized.
5 patients in the Johnson & Johnson trial were hospitalized.
Those small numbers make you feel less certain about the alleged 100% protection.
And the FDA document in the Moderna trial report a case of hospitalization in a patient who received the vaccine, even if they didn’t technically meet criteria for a hospitalized patient:
“One participant in the mRNA-1273 group, a participant >65 years of age who had risk factors for severe COVID-19, was hospitalized due to oxygen saturation of 88% on room air 2 months after receiving the second dose of vaccine. There was a verbal report of a positive SARS-CoV-2 RTPCR test 3 days prior to hospitalization; however, NP swab collected during hospitalization was negative for SARS-CoV-2. Due to absence of a confirmed RT-PCR result at the time of data snapshot, this case was not referred for adjudication and not captured. The pre-hospitalization RT-PCR result was later reported to be positive from an external CLIA-certified laboratory and may represent a severe COVID-19 case with hospitalization in the vaccine group.”
The bottom line here is that those numbers about vaccine efficacy that you’ve probably heard about - the Moderna vaccine is 94.1% effective, the Pfizer vaccine is 95% effective, and the Johnson & Johnson vaccine is 66% effective - are a bit misleading.
While the clinical trials are valuable, the real world data matters too
We already have published data from Israel to give us an insight into what happens when the Pfizer vaccine is given in the real world.
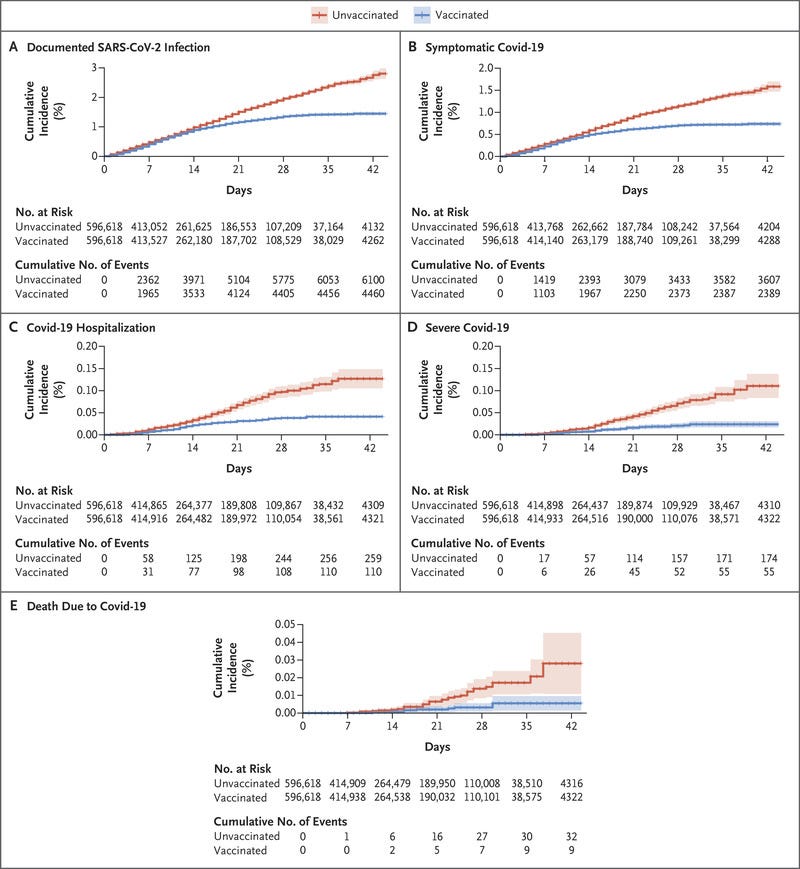
Let’s take a look below. I’m a huge fan of Kaplan-Meier curves because I think they visually demonstrate population-level medical information in an easily digestible way.
The graphs below have time on the horizontal axis and cumulative incidence on the vertical axis. The red line is an unvaccinated group the the blue line is the vaccinated group. Take a look at a number of different important endpoints:
We see here that the Pfizer vaccine certainly protects against death and hospitalization, but it isn’t perfect.
It’s vital to note that the total numbers here are really low (look at the scale of those vertical axes - they don’t go up anywhere close to 100%). But also vital to note that the numbers aren’t zero!
According to this real world data, the Pfizer vaccine is 87% effective at preventing hospitalization a week after the second dose.
Real world data from England demonstrates a similar story - significant protection against hospitalization and death, but it isn’t perfect.
I suspect that the numbers would be similar for the Moderna vaccine given it’s similar efficacy in the clinical trial coupled with its similar mechanism of action, but that’s just a conjecture and it’s not based in real world data.
What about reactions to the vaccine?
Another big variable that you might weigh is likelihood of having a reaction to the vaccine.
If you look at the presented data from the FDA documents, the Pfizer and Moderna vaccines have similar rates of fever after the second dose - 15.8% and 17.4%, respectively.
Johnson & Johnson has a slightly lower rate of fever, around 9%.
Some folks may take comfort in the fact that the J&J vaccine has a well-established mechanism of action, whereas the Pfizer and Moderna vaccines use novel mRNA technology. I suspect that we’ve had a long enough duration of follow up in clinical trials and the real world data to feel comfortable about the mRNA vaccine approach, but you may have a different level of comfort here.
Ease of use matters too
Only the J&J vaccine is a one-and-done shot.
The other two require a follow up injection, even if we may quibble about the timing and whether or not it’s even necessary.
So that’s certainly a point in favor of J&J.
And the freezer temperatures required by the two mRNA vaccines add a layer of complexity to the distribution, while J&J doesn’t need any dry ice.
And what about the variants?
This is a really big deal. Ultimately, it’s too soon to tell definitively here.
We know that the Johnson and Johnson vaccine was tested at a time where the B.1.1.7 and B.1.352 variants were circulating while the Pfizer and Moderna vaccines had completed their trials earlier. It’s far from a clear piece of evidence regarding protection, but it’s something.
There’s been a lot of in vitro testing of blood from people who received the Pfizer and Moderna vaccines to see if the new strains can be neutralized by these vaccines.
It seems that Pfizer likely provides some degree of protection against B.1.1.7, B.1.352, and P.1 and that Moderna may protect you from B.1.1.7 and B.1.352. While there are lots of reports about the lower levels of antibody titers against the variants, I’m not actually all that persuaded there’s any clinical difference.
You need to take these findings with a grain of salt since these experiments don’t actually tell us all that much since they don’t measure T cell activity and, more importantly, they don’t measure actual immunity in the real world (AKA the only thing that we actually care about).
So I haven’t seen anything to suggest that any variants are evading the vaccine response, but I haven’t seen anything that makes me feel certain that this is right.
It’s just too soon to know.
So what’s the bottom line?
I think all of these vaccines are great. I would recommend any of them.
Ultimately, we have the most robust data on the Pfizer vaccine both in the real world and in-lab studies against the different variants. It’s my first choice from a strict “how-confident-do-I-feel-in-the-data?” point of view.
Moderna seems to be fastest at reengineering their vaccine to create boosters with new strains in mind. But that doesn’t tell us anything about the current ones we have available. And even though this is the vaccine that I got, it’s probably not what I would choose if I had my pick of all three.
When it comes to comparisons here, I think there’s real value in the one-and-done approach of the J&J vaccine. It’s simple, you don’t have the time spent dreading the second dose reaction, and you don’t have to make any other appointments. Because of the ease of use, it’s probably the one I would pick right now if I were choosing, but I don’t feel all that strongly about that opinion.
At the end of the day, I think that deciding about these vaccines is like deciding about a type of exercise - the best one for you is the one that you’re willing to do.
And once you’ve gotten vaccinated, you have real protection against COVID. It’s not perfect, but it’s a huge step forward, and one that makes me feel comfortable about getting back to normal life.
Thank you for reading! If you’re enjoying my newsletter, please consider sharing with your friends and family and encouraging them to subscribe!
I always appreciate any feedback or thoughts you might have. You can reply directly to this email to reach me directly.