High blood pressure is often called “the silent killer,” but maybe it should be called the boring killer.
That’s because most cases of high blood pressure cause zero symptoms, but blood pressure is probably the most important modifiable risk factor for the development of heart attacks, strokes, kidney failure, and even dementia.
And in the information environment that we live in, hypertension1 doesn’t get very much attention.
Over the past week, I’ve had 4 different people ask me about skipping because Andrew Huberman did a segment on it, but zero people ask me about high blood pressure.
But whether or not we properly measure and treat blood pressure is way more important for your long term quality of life than whether or not you’re skipping to keep your joints supple and your muscles pliable.
I can’t tell you how many times I’ve had a patient ask me “do I really need to keep taking this blood pressure medication?” or negotiate about an end date for treatment.
Decisions about blood pressure management are incredibly common and impactful, even if they aren’t all that exciting.
So let’s tackle some of the most common blood pressure questions.
What causes high blood pressure?
For most people, the answer is that there isn’t one specific thing.
The most common culprits - too much body fat, too little physical activity, poor sleep,2 too much dietary sodium,3 - often coexist, so for many people, elevated blood pressure is multifactorial.
I like to think of high blood pressure as a mismatch between what our environment should be and what our environment actually is.
And so there is certainly some amount of dietary modification, weight loss, increased physical activity, better sleep, and stress reduction that will lead to remission of high blood pressure.
But the reality is that most people aren’t able to consistently adhere to these types of lifestyle adjustments.4
For every patient who has a surgically correctable cause of hypertension,5 there are dozens who just need to be medically treated.
What should blood pressure goals be?
The data is pretty clear that the lower our blood pressure is, the lower our risk of heart attack and stroke.
For every 20-point rise in systolic BP above 115, the risk of heart attack and stroke doubles.6
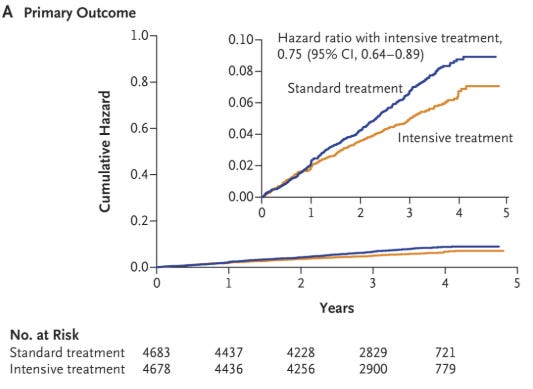
That comes from the epidemiologic evidence and it’s backed up by multiple high quality randomized controlled trials, including SPRINT and STEP.
Take a look at how cardiovascular outcomes improve over time with more intensive BP control in SPRINT:
Looks pretty similar to the benefit on cardiovascular outcomes seen in STEP:
And importantly, it seems that better blood pressure control even improves cognitive outcomes - there’s a suggestion that better treatment of hypertension lowers the risk of dementia.
But the SPRINT trial voluntarily took people off blood pressure medications, so doesn’t it overestimate the benefit of intensive blood pressure treatment?
One of the biggest criticisms of the most important clinical trial on hypertension management is that part of their treatment protocol had patients discontinue antihypertensive medications.
The protocol for that trial is here:
If patients were asymptomatic and had very well controlled blood pressure, their medical therapy was “stepped down” which means that blood pressure medications were taken away.
You can look at this in a couple of different ways.
The cynical interpretation of the trial is this study design sets up more intensive treatment to look better than less intensive treatment.
By taking asymptomatic patients who were doing well and removing blood pressure medications for no reason other than the trial protocol, you raise their blood pressure and thus their risk of complications of hypertension.
I used to think of this issue as a flaw in the study, but the longer I practice medicine, the more it seems that this represents what clinical practice is actually like.
Patients ask me *all the time* whether they can come off of blood pressure medications when their numbers are well controlled.
So this design of the SPRINT trial actually ends up being applicable to day to day clinical practice.
And, importantly, it tells us that if someone is doing well on their medications, we should stay the course.
When can you stop taking blood pressure medications?
This is one of the most important - and most common - questions that I get.
I think the answer is pretty simple.
Most people are probably undermedicated for high blood pressure and if your blood pressure is regularly elevated over 130/80, you should think about stepping up therapy rather than stepping it down.
The time to decrease blood pressure medications is when you are feeling lightheaded due to blood pressure being too low.7
And I think it’s really that simple.
When should we start medications for high blood pressure?
I tend to be aggressive with treating high blood pressure with a few exceptions:
A patient is actively making lifestyle changes - changing diet, exercising more, improving sleep
A patient is starting a GLP-1 agonist medication like Ozempic/Wegovy or Mounjaro/Zepbound
We are trying to figure out if there is a secondary cause of high blood pressure in a young person who is otherwise healthy
We’re uncertain if the blood pressure is truly high because we have very limited readings and we need to get more information
Someone has very labile blood pressure and is symptomatic with lightheadedness when their blood pressure is low
And that’s really it - I think that most people with elevated blood pressure should be started on medications if they aren’t immediately planning to institute lifestyle adjustments.
It’s way too easy to get into the pattern of “watch if for a few months” and then have a few months of elevated blood pressure turn into a few years of elevated blood pressure.
A few other things that should be considered
In no particular order, a few other pearls on high blood pressure:
Anyone who has high blood pressure and snores should probably be evaluated for sleep apnea, a major cause of difficult to treat high blood pressure
Ambulatory blood pressure monitoring is hugely valuable and helps figure out whether someone truly has high blood pressure when there is diagnostic uncertainty.
If someone still has high blood pressure on multiple medications, evaluating them for hyperaldosteronism is often illuminating - these patients also frequently have their blood pressure well controlled on a medication like spironolactone
Weight loss profoundly impacts blood pressure. Even losing as little as 5% of body weight often helps people get off medications
Medication choices for hypertension are different depending on other medical issues (in particular, things like diabetes, chronic kidney disease, and irregular heartbeats impact treatment choice)
Not having your blood pressure drop at night and during sleep (a non-dipping pattern) suggests higher cardiovascular risk
Taking a lot of NSAIDs - drugs like ibuprofen, Motrin, Advil, Aleve - tends to raise blood pressure
The hardest type of high blood pressure to treat is labile hypertension - where the pressure is sometimes really high and sometimes really low8
There is a surgical treatment for high blood pressure, but we’re still not sure if it really works
Renal denervation therapy - a procedure to interrupt signals from adrenaline to the kidneys - was a promising therapy for high blood pressure until the SYMPLICITY-3 trial showed that it was no better than pretending to do the procedure.
Subsequent studies have shown that newer devices probably lower blood pressure by about 6 mmHg.
These procedures have overall pretty unimpressive results, but that hasn’t stopped them from becoming FDA approved.
Ultimately, the list of patients who should receive this treatment is probably pretty small, and there are some pretty prominent skeptics of the therapy:
I know that this isn’t a fun or exciting topic, but it’s of vital importance
Blow off your own blood pressure at your own risk.
You might not feel your blood pressure creeping up but that doesn’t mean it’s harmless.
Keeping your blood pressure excellent lowers risk of heart attack, stroke, kidney failure, and dementia.
It doesn’t matter whether that’s done with drugs or with lifestyle changes - and it’s not a moral failing to end up on high blood pressure medications.
I often tell my patients that most heart disease prevention is blood pressure, cholesterol,9 and blood sugar10 management.11
That’s not flashy.
It’s not viral.
But it works.
So if you’re spending time perfecting your supplement stack or optimizing your sauna sessions, but your blood pressure is 142/88, then you’re missing the point.
Skipping is fine, but skipping your BP meds could kill you.
Hypertension and high blood pressure are the same thing. I’ll use them interchangeably.
Poor sleep in general can certainly cause high blood pressure, but undiagnosed and untreated sleep apnea is also a really big deal here.
Controversial, but there are certainly people who are sodium sensitive. Although some people in this space would argue that it’s not the sodium, per se, as it is the imbalance between sodium and potassium.
I often describe to patients that the amount of physical activity we should be doing goes up as we get older, but most people do less and high blood pressure is one of the consequences of that.
Something like renal artery stenosis, hyperthyroidism, or a tumor making cortisol, among others.
The degree of blood pressure elevation is important, but the length of time blood pressure is elevated for also matters.
That doesn’t mean you felt lightheaded one time when you were sitting for an hour and then got up quickly. It means feeling regularly lightheaded.
These patients often have high levels of stress and a pronounced response to environmental changes. They also often feel lightheaded when we treat high blood pressure. My treatment advise for these patients is to make sure they are sleeping, managing stress, and staying active. Aerobic exercise tends to help this group in my anecdotal experience.
Technically lipids.
Technically metabolic health and visceral fat.
And while that’s an oversimplification, it’s directionally accurate enough to make it a point worth emphasizing.