Fish oil: what is it good for?

Fish oil supplements are a huge business. We’re talking over $4 billion each year that Americans spend on fish oil.
As you might suspect, fish oil has a pretty high Q rating, both among patients and among doctors.
Lots of my patients who don’t like to take medicines are happy to take fish oil. After all, the list of potential benefits sounds pretty impressive: improved memory, lower blood pressure, reduced triglycerides, better mental health, anti-inflammatory, and the list goes on.
But you could be forgiven for being confused about whether fish oil is actually useful:
So what gives? Is fish oil good for you or is it bad for you? And does it cause atrial fibrillation?
Fish oil supplementation is one of the things I’ve changed my mind about over time.
Let’s take a look at the theory behind fish oil supplementation and then some of the clinical trial evidence. There’s a lot of information here, most of which is the context you need in order to interpret the data from clinical trials.
If you want to skip the explanation and just hear the bottom line, scroll down to the heading titled" “Enough with the explanation, just tell me the bottom line.”
Why did anyone think fish oil might help to prevent heart disease?
The rationale to use fish oil as a supplement to prevent or treat heart disease comes from an observation and a physiologic theory:
Inuits, who consume a diet rich in animal fat from marine sources (including fish oil), don’t seem to have much cardiovascular disease
The types of fats that humans consume has changed drastically over time in a way that’s hypothesized to increase risk of heart disease and consuming fish oil supplements may help to restore that balance
It’s worth noting that the observation that Inuits were actually free of cardiovascular disease may actually be more myth than fact.
And I’d also note that there’s controversy about whether or not the dietary change in fat consumption actually increases cardiovascular disease.
Unfortunately, we need to get into a tiny amount of nutritional biochemistry
There are 3 major macronutrients that we eat: fats, carbohydrates, and protein. You could include alcohol in there as a 4th macronutrient, but that’s a conversation for another newsletter.
There are only two fats that are considered “essential” for our diet, which means our bodies need them to function and can’t make them from other sources.
Alpha linolenic acid (ALA) - an omega-3 fatty acid
Linoleic acid - an omega-6 fatty acid
The balance between omega-3s and omega-6s may influence heart disease risk factors like inflammation and blood clotting and this balance has changed over time.
Now, ALA isn’t really the active omega-3, you need EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) to do the biologic work.
ALA is found in plant sources like flaxseeds, walnuts, and chia seeds - when you hear that these have a reputation as superfoods, it’s likely because of their ALA content.
ALA can be converted into EPA and DHA, but only at about 5% efficiency, so you’re going to struggle to get adequate amounts of EPA and DHA just through plant sources. Which may mean that the plant-based on omega-3 sources aren’t quite as super as some of the hype might suggest.
EPA and DHA come from fish, or, more precisely, from the algae that fish eat. That’s why algae oil shows promise as a vegan omega-3 supplement, even if its extraction can be challenging.
The next step - more links between fish and heart health, and not just Inuits
There’s enough evidence on fish consumption that a recommendation to eat more fish made its way into the cardiovascular prevention guidelines.
There’s a ton of observational data in lots of different groups making the connection that fish consumption is associated with better cardiovascular health.
But remember - this is nutritional epidemiology, so these links don’t prove anything at all. Just because there’s a possible mechanism and epidemiologic evidence to suggest a connection doesn’t actually tell us anything definitive.
The road to hell is paved with biologic plausibility.
And we can’t forget that there’s a difference between eating fish and taking fish oil.
There have been a ton of clinical trials looking at fish oil supplements
It’s challenging to make sense of all the clinical trials because the interventions and outcomes measured aren’t the same in all of these studies.
Some of them tested combinations of EPA and DHA. Some of them tested EPA or DHA alone. Many tested different doses. They all looked at slightly different patient populations.
Some of the trials looked at blood markers of cholesterol or triglyceride levels. Some of the trials looked at actual heart attacks and strokes.
There were also a number of different placebos compared to the fish oil, which is an important point that I’ll emphasize again later.
And, as you might expect from a mixed bag of studies, there’s a mixed bag of results.
The most impactful of these trials is REDUCE-IT, which I’ll talk about in the section below. Here’s a tl;dr for the other big ones:
MARINE - lower lipid numbers with EPA, no data on heart attacks
ANCHOR - improved lipids with EPA, no heart attack data
GISSI - mix of DHA and EPA, 10% reduction in cardiac events
JELIS - high dose EPA, small reduction in cardiac events
ORIGIN - mix of EPA/DHA in diabetics, no impact on heart attacks
ASCEND - mix of EPA/DHA in diabetics, no reduction in heart disease
VITAL - mix of EPA/DHA, no impact on heart disease
STRENGTH - DHA alone, no reduction in heart disease
So now let’s talk about REDUCE-IT, the most impactful fish oil trial that we have
REDUCE-IT has very impressive top-line results. Just look at the event curves:
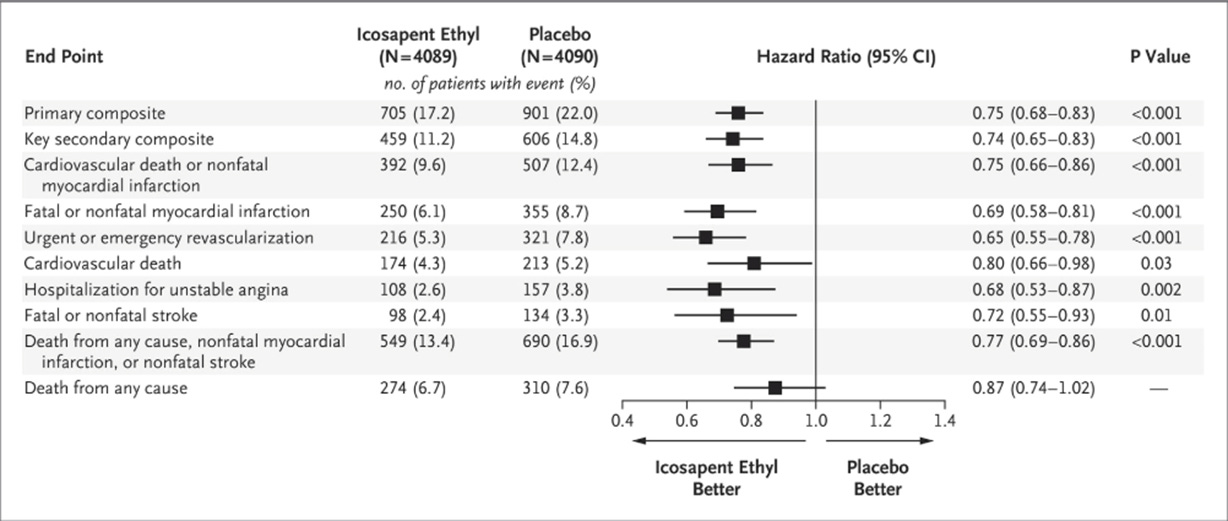
This study gave patients either high dose purified EPA (AKA icosapent ethyl, brand name = Vascepa, which comes from vascular EPA) or a mineral oil placebo.
There are two important differences between REDUCE-IT and a lot of the other trials:
REDUCE-IT used a much higher dose of purified EPA than the other studies
REDUCE-IT looked at patient who had established cardiovascular disease and elevated triglycerides, so it’s a sicker group than a lot of the other trials. Studying sicker patients means you’re more likely to find an effect size, since bad outcomes happen more frequently to people who are already sick
They found very impressive results. Vascepa reduced the risk of basically every single important outcome:
On the surface, it seems like EPA is a miracle drug.
But as you into the trial a bit further, you see that mineral oil (the placebo in this study) actually impairs absorption of statins, which are pretty incredible drugs at reducing heart disease.
In the supplementary appendix for this trial, you can see that the placebo group had a rise in their LDL-cholesterol, their apolipoprotein B, and their high sensitivity CRP (a marker of inflammation):
Something’s fishy here!
So was REDUCE-IT a trial that showed a reduction in cardiovascular events with EPA, or was it a trial that showed an increase in cardiovascular events when you withdraw statin therapy?
I would argue that this can’t prove a benefit of EPA compared to placebo, since a placebo wasn’t used. So, in my view, we’re left more confused than when we started.
There’s also the issue of quality of fish oil supplements - what you see isn’t necessarily what you get
I don’t think that Vascepa (or prescription icosapent ethyl) is harmful, but I’m concerned about ove-the-counter fish oil for two reasons:
I worry about purity - are you actually getting EPA/DHA in the ratios that they advertise on the bottle? Usually you are, but not always.
These are unstable fatty acids prone to oxidation based on their chemical structure if storage conditions aren’t right. If these become oxidized, they may promote heart disease. Usually oxidation levels are low, but not always.
These products are usually going to be fine if you buy from reputable sources, but as with all supplements, there’s a bit of a gamble whenever you buy something that isn’t regulated.
Enough with the explanation, just tell me the bottom line
I’ve changed my mind on fish oil as I’ve had time to analyze REDUCE-IT. I used to recommend taking high dose EPA to my patients, and I have prescribed quite a bit of Vascepa.
But as I dig into the data more, I’m less convinced about the size of the benefit. I think that there’s a decent chance that EPA taken at REDUCE-IT or JELIS dosing helps reduce heart disease, but I also don’t think that this is proven.
I think that eating fish is probably good for your heart.
Mineral oil is bad for you, and you shouldn’t consume it.
The personalized future here may be to measure your red blood cell omega-3 levels and decide on fish consumption and EPA supplementation based on your own biomarkers rather than crudely extrapolating heterogeneous clinical trial data.
So I’m going to leave you with a murkier conclusion than I’d like here, but the data show what they show.
Thank you for reading and subscribing! Please share freely with friends and family and encourage them to subscribe!