One of the odd things about medicine is that sometimes our most common practices often lack a strong evidence base.
There’s a meme in medicine called “things we do for no reason” to describe this tendency for a practice to become ingrained into the culture of what we do in the hospital even when we haven’t generated great evidence to support that practice.
And it might surprise many non-medical readers to know that when doctors are trained and become part of the guild of medicine, we frequently carry on these practices without ever asking about the evidence to support them.
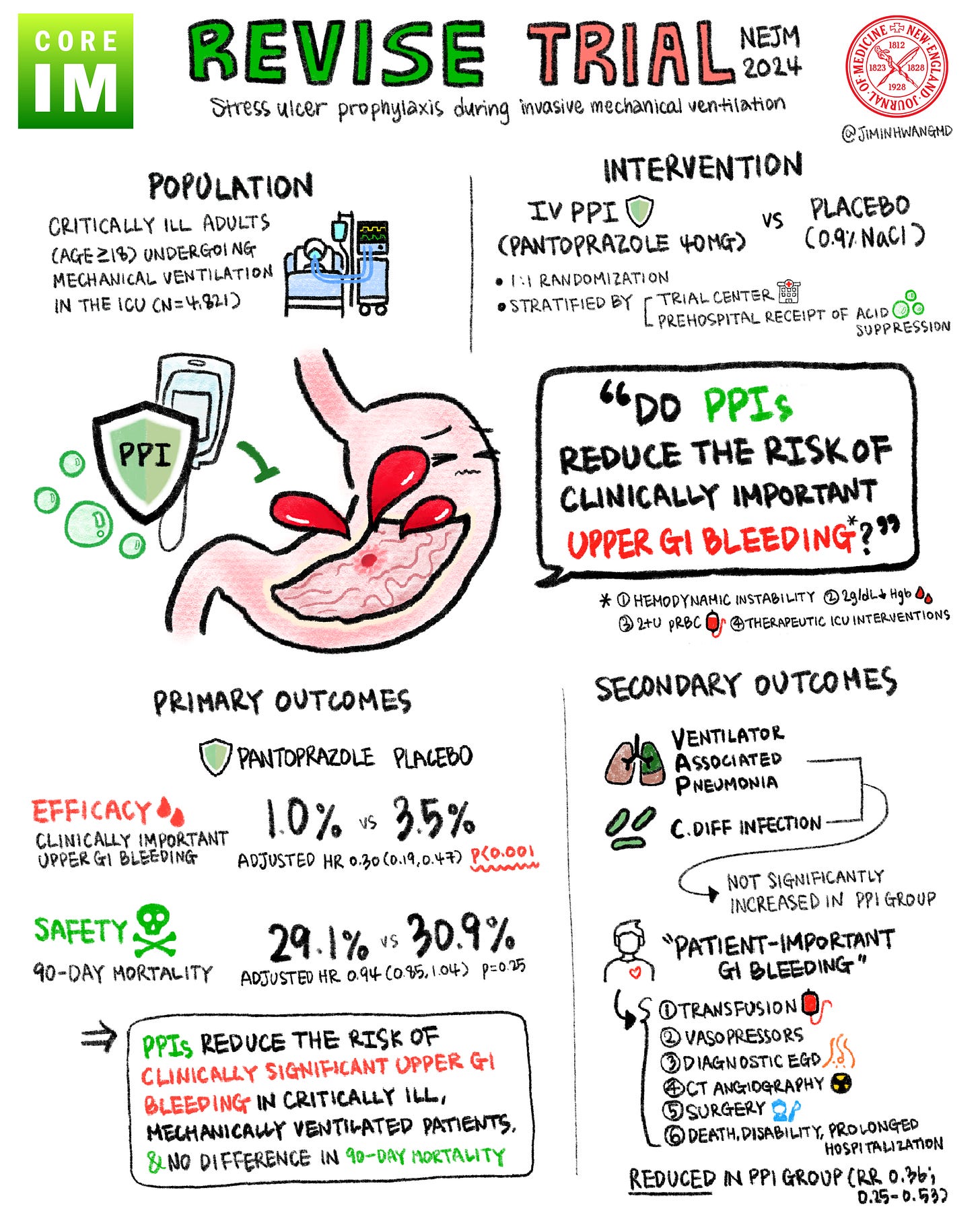
We recently released another episode in our Beyond Journal Club Podcast looking at a topic that will feel like inside baseball to anyone who isn’t involved in medicine: the use of acid suppressing medications in the intensive care unit for intubated patients.
This episode looks at the REVISE trial in detail - it’s a study evaluating a practice that almost everyone who has ever worked in the hospital is intimately familiar with.
Patients who are critically ill are at risk for a lot of bad things to happen while they’re hospitalized, and these patients are often really complicated.
As a consequence, most ICUs operate with an ICU checklist of automatic things that are discussed everyday - things like preventing blood clots, mobilization, feeding, and preventing stomach ulcers.
This podcast looks at the evidence behind preventing ulcers in critically ill patients.
I started out not being really sure if the practice of trying to prevent ulcers in the ICU was one of those things we do for no reason.
But thankfully, after I dug into the evidence, it seems to me that this is a pretty reasonable practice - giving medication to reduce ulcer formation improves outcomes that patients care about.
Working on the podcast also inspired me to try to ask the question “how good is the evidence for this thing that I do all the time” more frequently.
It’s often some of the most common - and the most mundane - questions in medicine that we don’t have great answers to.
We owe it to our patients to be consistently demanding that the evidence base supporting our decision making is strong and we should be comfortable thinking that our clinical practices should have an expiration date, especially as medicine and technology change the context in which we perform them.
In the podcast, you’ll learn about:
How common are stress ulcers in the GI tracts of critically ill patients?
What is “clinically important bleeding?”
What are risk factors for stress ulcer bleeding in ICU patients?
The evidence behind the use of medications like PPIs and H2 blockers for preventing stress ulcers
A deep dive into the REVISE trial
A detailed discussion of whether these results apply to all ICU patients or we should be excluding the sickest ones
I hope you enjoy!