I’ve written before about the adage that half of what you learn in med school will be wrong in 20 years, the problem is that you don’t know which half.
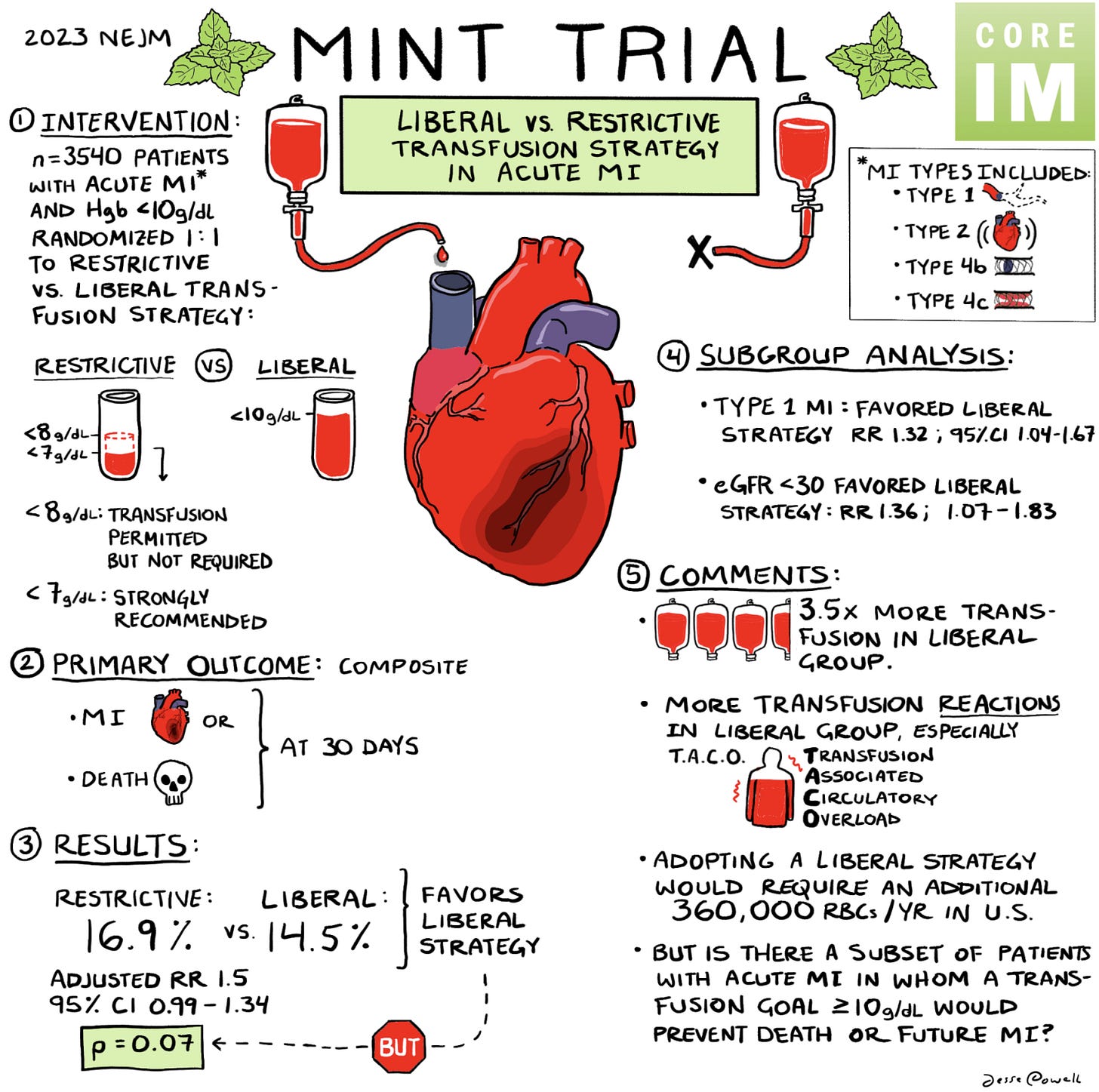
And that adage is particularly applicable to blood transfusions, where the question of how much blood to transfuse in a patient is a really tough one to answer.
Blood transfusions have undergone a pretty astounding paradigm shift1 over the last generation - most doctors practicing today would say that when it comes to blood transfusions, less is almost always more.
While we used to transfuse patients pretty liberally, a series of trials over the last 25 years have established that a liberal transfusion strategy isn’t better for most really sick patients.
I wrote about this question a few months ago, wondering “Why was I wrong about blood transfusions” when I dove into the MINT trial in detail.
For the latest episode of our Beyond Journal Club podcast series, we tackled this trial in audio form, diving a bit more deeply into the data and biology.
We interviewed two of the lead investigators from the trial, Jeffrey Carson and Sunil Rao, as part of the prep, and some of their clips are in the podcast.
In the podcast, we cover:
Why blood transfusions make sense, but also why they might be risky
What makes a blood transfusion decision during a heart attack different than a decision in other clinical scenarios
The history of blood transfusion trials
The MINT trial in detail with a look at the protocol and results in depth
What we should all take away from this trial.
You can review the show notes in detail here. Below is our graphic on the landmark blood transfusion clinical trials.
I hope you enjoy!
I’ll ignore the initial history of bloodletting (the opposite of transfusion), which was popular in a different era in medicine. It’s hypothesized that bloodletting may have contributed to George Washington’s death.