I wanted to take today’s newsletter to share a new Beyond Journal Club podcast episode looking at a trial asking about the length of time someone should be on antibiotics when they have bacteria in their bloodstream (medical term: bacteremia).
It’s a common problem to see in the hospital - someone gets admitted with an infection, and when we culture their blood, we see bacteria in there.
This can be a scary situation, and the impulse of many doctors is that longer is better when it comes to antibiotics in these cases.
For a while, evidence has been accumulating that a shorter course of antibiotics might be just as good as a longer one, albeit in small trials rather than big ones. But the direction of the evidence has been pretty consistent.
The BALANCE trial, recently published in NEJM is the largest study ever done on antibiotic duration for bacteremia.
I’ll skip to the top line result quickly - shorter courses of antibiotics seem just fine in most cases.
But if you’re just asking the question “is a 7 day course of antibiotics in bacteremia good enough, then you’re asking the wrong question.
Or, at least, you’re asking an incomplete question.
The most notable thing that I heard when preparing for this podcast came from one of the ID doctors we interviewed,1 who told us:
“I feel somewhat uncomfortable discussing bacteremia as a generalizable thing divorced from nuances.”
That’s the most important point in the podcast.
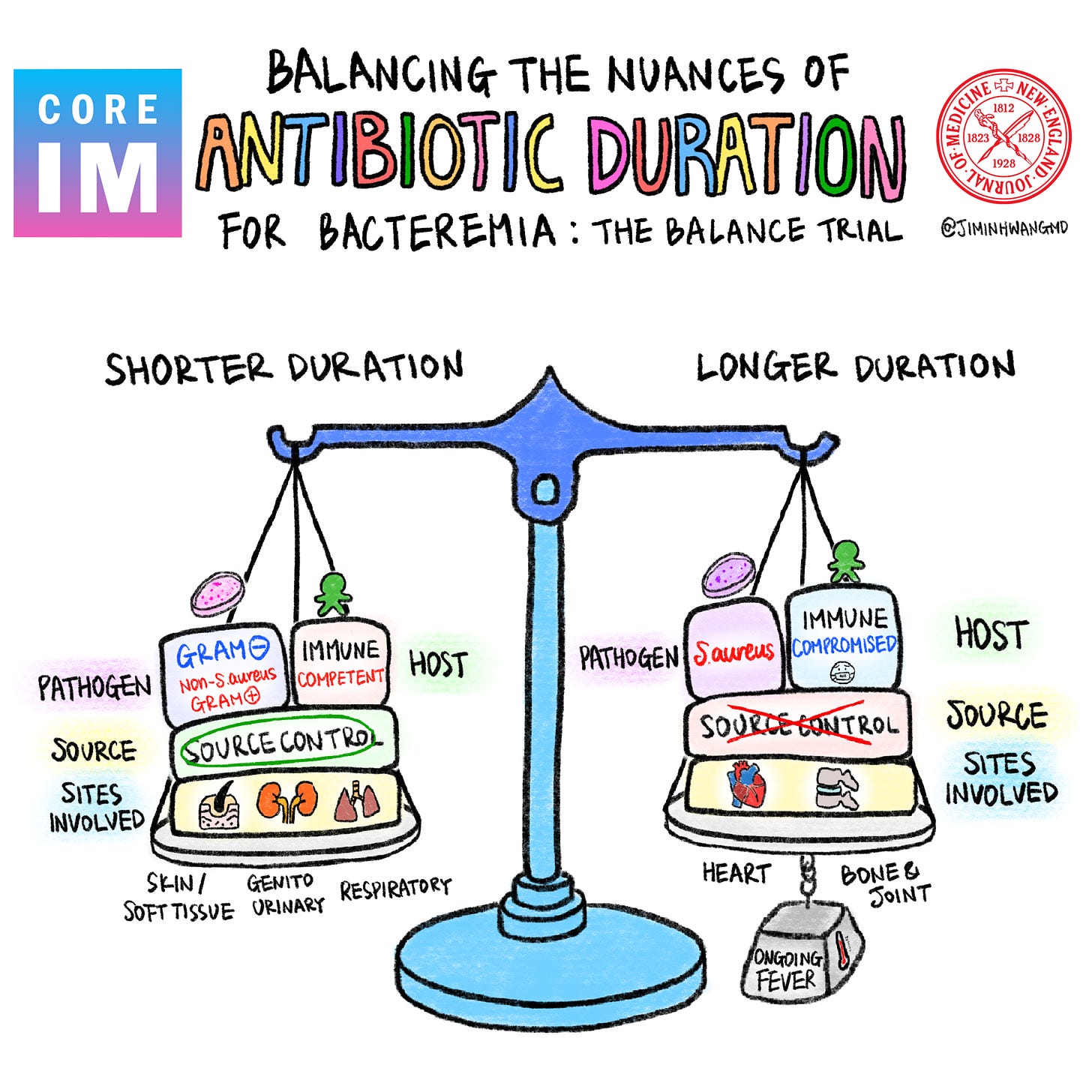
Asking “how long should antibiotics last?” without specifying the host, organism, and source means that you’re asking an unanswerable question if you want to take good care of the patient.
That clinical context really matters.
A Better Bacteremia Framework
Like many problems in medicine, antibiotic duration for bacteremia is a fractal problem.
Each question you need to answer has a whole bunch of downstream questions that also need to be answered, otherwise you’re making a decision without considering the entire picture.
Before you can meaningfully talk about antibiotic duration for bacteremia, you need to think about three things:
The Host: Are they hemodynamically stable? Do they have hardware? Are they immunocompromised? How quickly did they improve?
The Organism: Staph aureus behaves completely differently than E. coli. Strep viridans carries different endocarditis risk than Strep pyogenes.
The Source: Was source control obtained? Is there osteomyelitis? What about endocarfitis? Cellulitis vs. abscess makes a difference too.
The episode walks through each of these in detail, with concrete clinical examples of when you’d lean toward 7 days versus when you’d be thinking a longer duration makes more sense despite what the trial says.
What This Trial Actually Shows
BALANCE randomized patients with various types of bacteremia to either 7 or 14 days of antibiotics. Most had uncomplicated gram-negative bacteremia,2 but about 20% had gram-positive organisms.
The 7-day arm had a mortality rate of 14.5% versus 16.1% in the 14-day arm. Non-inferior.
Secondary outcomes like ICU admission, relapse, C. diff, length of stay were all similar between groups.
The median treatment in the “7-day” arm was about 8 days because clinicians were making individualized decisions based on patient factors, organism characteristics, and clinical response, which is exactly what we should be doing.
Paradigm Reinforcing, Not Paradigm Changing
This is one of those trials that doesn’t upend clinical practice but rather confirms that the evidence has been nudging us in the right direction.
A trial doesn’t have to have a surprising result to be important. It’s really reassuring to know that those smaller studies haven’t been misleading us.
We’ve already had trials showing shorter courses work for ventilator associated pneumonia, pyelonephritis, community acquired pneumonia, cellulitis, intra-abdominal infections.
BALANCE adds bacteremia to that list with the largest patient cohort we’ll probably ever see.
What this means to me is that the default should now be 7 days of antibiotics for uncomplicated gram-negative bacteremia in immunocompetent patients.
But you still need to individualize treatment. It’s important not to be too concrete about a trial result like this. Longer courses are still warranted for:
Staph aureus bacteremia
Endocarditis
Osteomyelitis
Persistent fever despite appropriate antibiotics
Immunocompromised hosts
Inadequate source control
Why This Trial Matters Even If It’s “Expected”
One of my co-hosts asked: if we already suspected these results, was this trial worth the resources?
My answer: absolutely yes.
There’s a huge difference between “we think this is probably true” and “we feel much more confident that this is true based on robust data.”
Small trials can point in one direction, then a large trial in the modern era comes along and completely reverses what we thought we knew. (Think MINT trial on transfusion thresholds, which we covered in a previous episode.)
BALANCE reassures us that the direction of the evidence has been correct and we don’t need to backtrack.
Listen If You Want to Actually Understand This Trial
The episode is worth your time because we go deep on the nuances that get lost when people just quote the headline.
We discuss:
Which organisms weren’t included (HACEK, TB, Listeria, Capnocytophaga, Staph aureus)
How to think about gram-positives in this trial
The difference between trials that change paradigms versus trials that reinforce them
Why antibiotic stewardship needs these kinds of large confirmatory studies
Listen wherever you get your podcasts, or read the full transcript here.
I’d love to hear your thoughts, especially if you’ve been in situations where the “right” antibiotic duration wasn’t obvious and you had to BALANCE (sorry, couldn’t resist) competing considerations.
Thank you for reading! Please share with friends and family and encourage them to subscribe!
Disclaimer: This is my opinion, not medical advice. Reading this newsletter does not constitute the formation of a doctor-patient relationship and is no substitute for the opinion of your doctor.
The process for these podcasts usually involves talking to more than 10 different specialists about the trial results, so they are heavily informed by people with significant clinical expertise and experience.
The majority were E. coli UTI sources